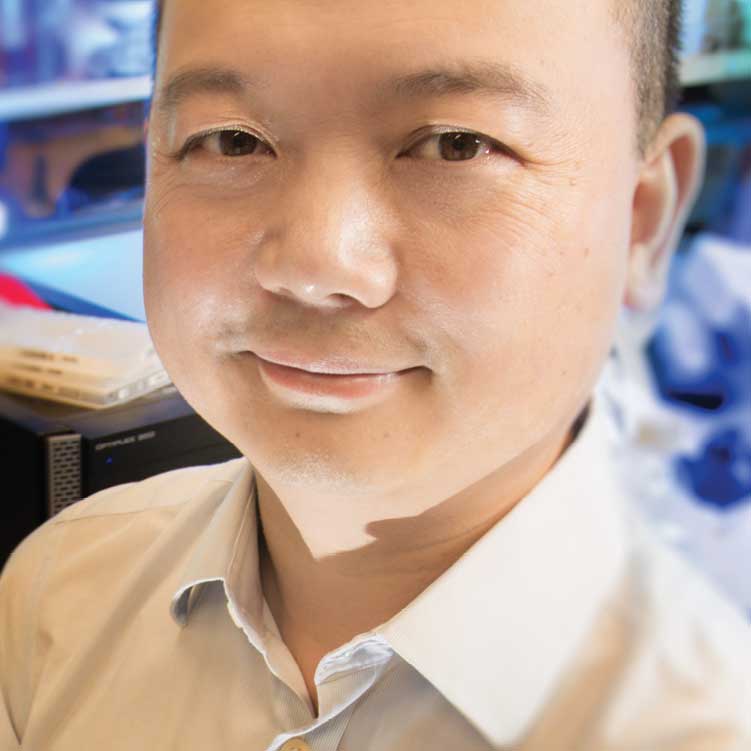
Tapping our Immune System's Superpower An interview with Ye Zheng
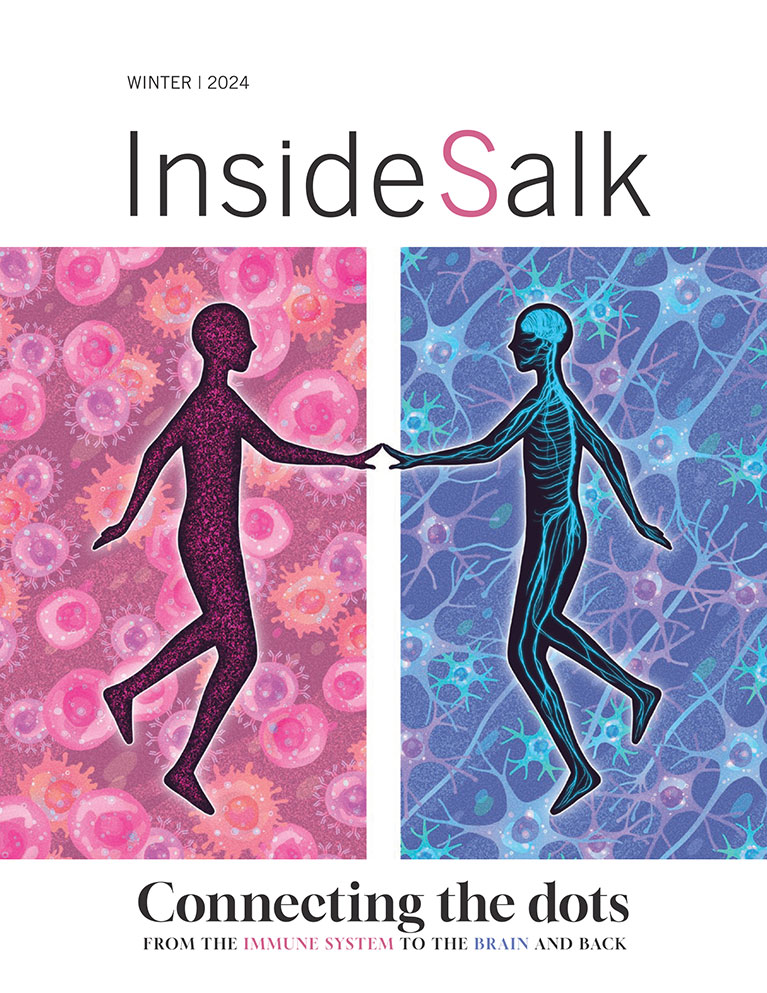
We all have a superhero—or supervillian—inside our bodies. It’s called our immune system. Every day, a healthy immune system repels a host of adversaries—bacteria, viruses, parasites—you name it! But it can also go berserk, resulting in multiple sclerosis, rheumatoid arthritis and other autoimmune disorders.
Its powers to heal or harm don’t stop there. Ye Zheng, associate professor in the Nomis Foundation Laboratories for Immunobiology and Microbial Pathogenesis, says that immunology is a rapidly expanding field with a direct impact on people. Scientists are discovering that the immune system is entwined with additional diseases such as autism, cancer and diabetes. If they can decipher the links between the immune system and these diseases, they may have a whole new weapon to maintain human health.
In a conversation with Inside Salk, Zheng shares his hopes and his hesitations about tapping our immune system’s superpower in ways not even imaginable just a few years ago.
What do people misunderstand about the immune system?
People make the mistake of thinking that the immune system deals solely with infectious diseases. But it’s much more than that. It’s always on duty, performing regular cleanup of bodily waste, such as dead cells. A lazy immune system that allows waste build-up leads to chronic inflammation. And inflammation underlies many diseases. In my lab we’re asking questions such as: How exactly does the immune system interact with chronic inflammatory diseases? And how can we correct this? It is a less developed segment of immunology. There is still much to learn.
Did you always want to be an immunologist?
Not really. It sort of happened by accident. I grew up in Beijing, where my parents were electrical engineers, and early on I was good with science and math problems. In fact, when I was in high school, I was chosen to be on China’s four-person entry in the International Chemistry Olympiad. We won the gold medal. I earned my PhD in biological sciences at Columbia University and then, with a postdoctoral fellowship, conducted research in the lab of immunologist Alexander Rudensky, first at the University of Washington in Seattle and later at Memorial Sloan Kettering Cancer Center in New York City. I like immunology because it’s a very large, very interesting field and also very helpful to people.
What do you enjoy doing outside the lab?
I love nature—camping and hiking. I especially liked living in Seattle where there is such a variety of terrain: mountains, ocean, islands. A change of environment is very good for stimulating your thinking. My wife, Yang Dai, also loves the outdoors. We have a 16-month-old daughter, Marissa, and we just bought a larger van so that we can go camping together.
What is the most surprising advancement in immunology?
Through human genetic mapping, we are finding a surprising overlap between genes linked with disease and genes linked with immune system function. Our hope is that, with a better understanding of this relationship, we can find additional ways to intercept and treat diseases.
Former President Jimmy Carter made headlines last year when immunotherapy was used, apparently successfully, to treat his melanoma. Are you excited about the prospects of using the immune system to fight cancer?
I’m excited but also cautious about making the promise that the immune system can cure cancer. We are not there yet, at least not for the majority of the cancer patients today. I believe the most benefit to cancer patients will come from a combination of immunotherapy and other standard treatments.
The problem is this: While immune cells can be trained to kill cancer cells—you risk them continuing their attack on other parts of the body. It can cause autoimmune disease, and even be lethal. There must be a balance when you turn the power of the immune system loose; there has to be some sort of check.
What would you like to know about the immune system in the next five to ten years?
Two things: one is more about tumor immunology and immunotherapy. The problem right now is that you can have two people with the same type of tumor yet the prescribed therapy only works on one person. What can we do to change that?
The second subject is neurological disorders, such as autism and Alzheimer’s, where there aren’t really any highly effective drugs. If we can develop more mechanistic insight into how immune cells play a role in these disorders then we can do something about it.
“Through human genetic mapping, we are finding a surprising overlap between genes linked with disease and genes linked with immune system function. Our hope is that, with a better understanding of this relationship, we can find additional ways to intercept and treat diseases.”
What is the focus of your lab in the immunology field?
In my lab we focus on immune cells called Tregs. They help regulate the more aggressive immune cells, telling them when to pull back from attack. A protein called Foxp3 plays a key role within Treg cells and we recently discovered a articular genetic sequence in this gene that is responsible for the stability of a Treg. Being able to manipulate Tregs into strengthening or quieting the immune response could lead to ways to treat autoimmune diseases as well as attack cancer cells.
You’re collaborating with Salk Professor Ronald Evans on yet another newly identified role for the immune system: its effect on metabolism. What are you learning?
Yes, this is another emerging field called immunometabolism. We are studying how immune cells interact with fat cells to regulate energy storage and consumption. People think that fat is static but it isn’t. Fat has so many immune cells it almost looks like an immune organ. A few months ago Ron and I discovered how immune cells were causing diabetes in aged, lean mice. We’re calling it a new disease: type 4 diabetes. This discovery could have real impact for our aging population.
Support a legacy where cures begin.
Featured Stories
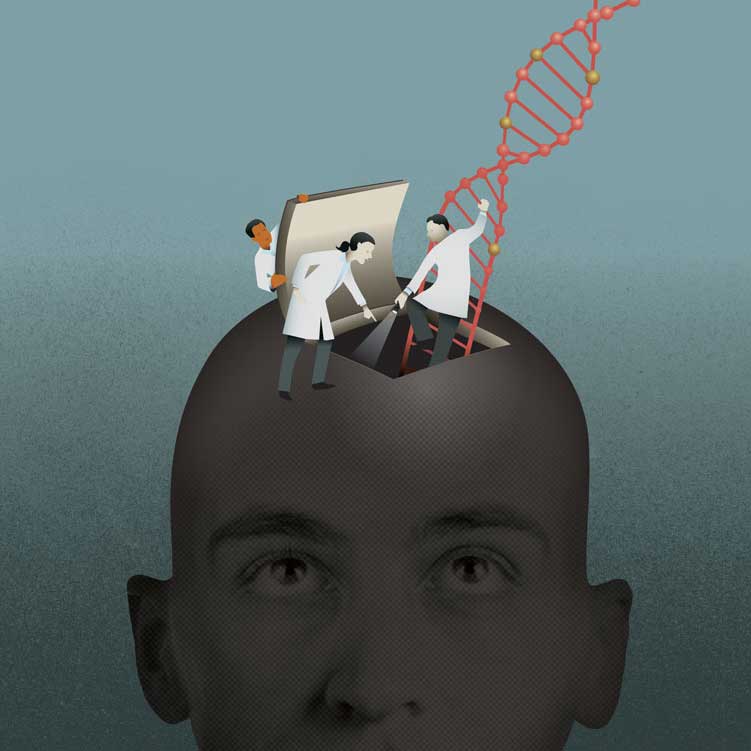 Beyond DNA: Unlocking the Secrets of the EpigenomeA layer of regulatory information on top of DNA is proving to be as important as genes for development, health and sickness.
Beyond DNA: Unlocking the Secrets of the EpigenomeA layer of regulatory information on top of DNA is proving to be as important as genes for development, health and sickness.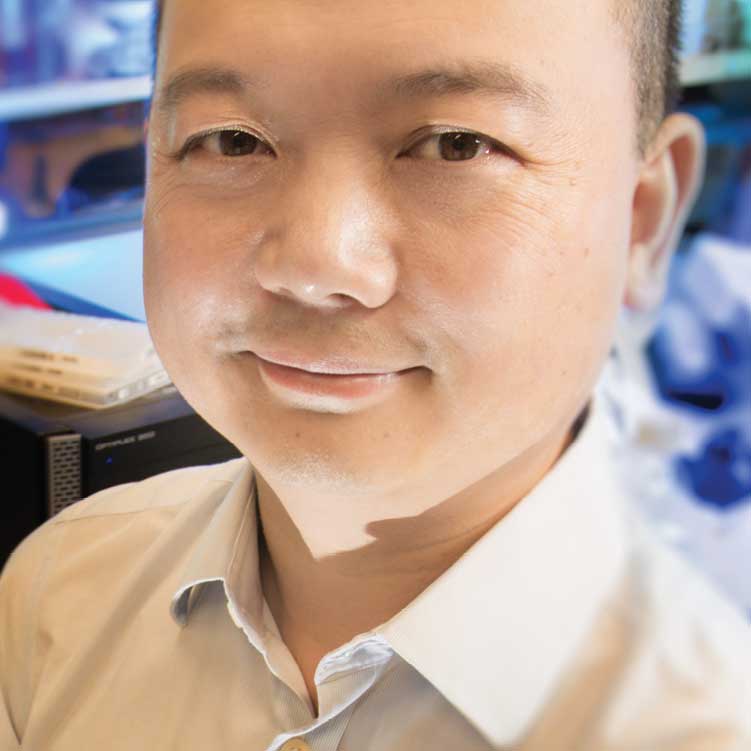 Tapping our Immune System’s SuperpowerWe all have a superhero—or supervillian—inside our bodies. It’s called our immune system. Every day, a healthy immune system repels a host of adversaries—bacteria, viruses, parasites—you name it!
Tapping our Immune System’s SuperpowerWe all have a superhero—or supervillian—inside our bodies. It’s called our immune system. Every day, a healthy immune system repels a host of adversaries—bacteria, viruses, parasites—you name it! All about town with Pablo HollsteinGrowing up in Quito, Ecuador, Pablo Hollstein was passionate—and precise —about science from an early age.
All about town with Pablo HollsteinGrowing up in Quito, Ecuador, Pablo Hollstein was passionate—and precise —about science from an early age.