Pancreatic cancer has the highest mortality rate of all major cancers. It is especially difficult to treat because the tumors grow so quickly and are constantly evolving. But patient-derived organoids could change all that. In this emerging biotechnology, researchers obtain a small sample from a patient biopsy and use it to grow 3D tissues in the lab. These “organoids” act as miniature models of the patient’s pancreatic tumor and can be used to quickly evaluate which cancer drugs might work best for them. A recent study by Assistant Professor Dannielle Engle, postdoctoral researcher Jan Lumibao, and colleagues provided critical insights into the robustness of patient-derived organoids as a clinical model of pancreatic cancer. They found the organoids’ gene expression and drug responses were not affected by the brand of extracellular matrix used in the cell culture. Data like this increases confidence that clinical conclusions are reliable across different labs and batches of organoids. They also identified one matrix brand that sped up the growth of tumor organoids, making it particularly well-suited for the fast pace of pancreatic cancer treatment protocols.
Read News ReleaseCancer
This time, it’s personal: Enhancing patient response to cancer immunotherapy
Immunotherapy has revolutionized the way we treat cancer in recent years. Instead of targeting the tumor itself, immunotherapies work by directing patients’ immune systems to attack their tumors more effectively. Still, fewer than half of all cancer patients respond to current immunotherapies, creating an urgent need to identify biomarkers that can predict which patients are most likely to benefit. Associate Professor Diana Hargreaves, postdoctoral researcher Matthew Maxwell, and colleagues have done just that, revealing that mutations in a gene called ARID1A make patients more likely to respond positively to immune checkpoint blockade—a type of immunotherapy that works by keeping cancer-fighting immune cells turned “on.” The ARID1A mutation prompts an antiviral response that pulls more cancer-fighting immune cells into the tumor, and because the gene is present in many cancers—endometrial, ovarian, colon, gastric, liver, and pancreatic—the biomarker could have a huge impact on identifying patients for specific immunotherapies. The findings also encourage the development of drugs that target ARID1A and related proteins as a way of sensitizing other tumors to immunotherapy.
Read News ReleaseLung cancer hijacks immune cell metabolism to fuel its own growth
Lung adenocarcinoma is the most common lung cancer and the cause of most cancer-related deaths in the United States. There are several ways lung adenocarcinoma can arise, one of which involves a mutation in a protein called EGFR (epidermal growth factor receptor). Modern immunotherapies don’t work against EGFR-driven lung adenocarcinoma, and while other types of lung cancer drugs do exist, patients typically become resistant to them within a few years. Professors Susan Kaech and Christian Metallo, alongside Salk colleagues and collaborators at Yale University and UC Los Angeles, discovered that EGFR-driven lung adenocarcinoma hijacks immune cells called macrophages, pulling them into the tumor and turning them into cancer fuel suppliers. The findings could inspire new lung adenocarcinoma interventions that disrupt this tumor cell-macrophage relationship. They also suggest that treatments using EGFR inhibitors may be more successful when paired with statins, a class of drugs commonly used to lower cholesterol levels.
Read News ReleaseFeatured Stories
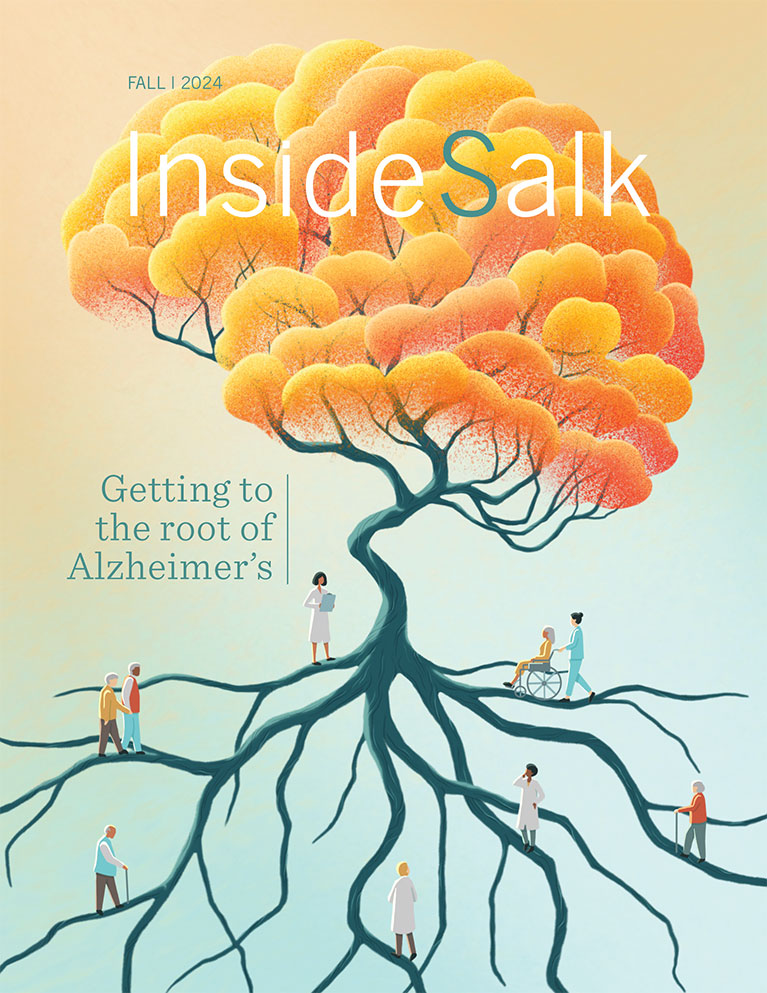
 Getting to the root of Alzheimer’sSalk scientists are teaming up to understand brain aging. By collaborating across disciplines like genetics, neuroscience, and immunology, our researchers are uniquely positioned to lead us into a future of healthier aging and effective therapeutics for Alzheimer’s.
Getting to the root of Alzheimer’sSalk scientists are teaming up to understand brain aging. By collaborating across disciplines like genetics, neuroscience, and immunology, our researchers are uniquely positioned to lead us into a future of healthier aging and effective therapeutics for Alzheimer’s. Salk mourns the loss of Joan JacobsThe Salk Institute lost one of its greatest supporters and one of San Diego’s most generous philanthropists when Joan Jacobs died on May 6, 2024, in La Jolla, California. She was 91 years old.
Salk mourns the loss of Joan JacobsThe Salk Institute lost one of its greatest supporters and one of San Diego’s most generous philanthropists when Joan Jacobs died on May 6, 2024, in La Jolla, California. She was 91 years old. Axel Nimmerjahn— Widening perspectives through plane windows and microscope lensesInside Salk sat down with Nimmerjahn to hear how he went from curious child to world renowned researcher. Now a professor at Salk, he studies the central nervous system and designs new tools—like mini microscopes!—to study the system's various cell types.
Axel Nimmerjahn— Widening perspectives through plane windows and microscope lensesInside Salk sat down with Nimmerjahn to hear how he went from curious child to world renowned researcher. Now a professor at Salk, he studies the central nervous system and designs new tools—like mini microscopes!—to study the system's various cell types. Jálin Johnson— Enhancing equity and inclusion at Salk and beyondOver the course of nearly 30 years dedicated to advocacy work, Jálin B. Johnson has served those in need and has given a voice to the voiceless—a principle that has guided her throughout her career. This commitment continues to shape her work as she steps into the role of director of Salk’s Office of Equity & Inclusion.
Jálin Johnson— Enhancing equity and inclusion at Salk and beyondOver the course of nearly 30 years dedicated to advocacy work, Jálin B. Johnson has served those in need and has given a voice to the voiceless—a principle that has guided her throughout her career. This commitment continues to shape her work as she steps into the role of director of Salk’s Office of Equity & Inclusion. Lara Labarta-Bajo—An immunologist’s journey from Barcelona and ballet to the brainWhether dancing in Spain or surfing in San Diego, Lara Labarta-Bajo has always celebrated the power of the human body. Now a postdoctoral researcher in Associate Professor Nicola Allen’s lab at Salk, she studies how the immune system connects the body to the brain and how this relationship evolves as we age.
Lara Labarta-Bajo—An immunologist’s journey from Barcelona and ballet to the brainWhether dancing in Spain or surfing in San Diego, Lara Labarta-Bajo has always celebrated the power of the human body. Now a postdoctoral researcher in Associate Professor Nicola Allen’s lab at Salk, she studies how the immune system connects the body to the brain and how this relationship evolves as we age. Professor or partner? Luc Jansen’s switch from science to lawDashed dreams of medical school brought Jansen to Salk's campus back in 2003, where he simultaneously contemplated a career in scientific research and a career in big law. Though he decided on law in the end, Jansen's affection for Salk remains as he now hosts Salk gatherings in his New York City office and excitedly shares the enduring importance of basic science.
Professor or partner? Luc Jansen’s switch from science to lawDashed dreams of medical school brought Jansen to Salk's campus back in 2003, where he simultaneously contemplated a career in scientific research and a career in big law. Though he decided on law in the end, Jansen's affection for Salk remains as he now hosts Salk gatherings in his New York City office and excitedly shares the enduring importance of basic science. Rising Stars and DISCOVER programs provide new opportunities for trainees from underserved backgroundsThe Salk Institute recently hosted two inaugural events designed to enhance diversity within the scientific community: the Rising Stars Symposium and the Diverse Inclusive Scientific Community Offering a Vision for an Ecosystem Reimagined (DISCOVER) Symposium.
Rising Stars and DISCOVER programs provide new opportunities for trainees from underserved backgroundsThe Salk Institute recently hosted two inaugural events designed to enhance diversity within the scientific community: the Rising Stars Symposium and the Diverse Inclusive Scientific Community Offering a Vision for an Ecosystem Reimagined (DISCOVER) Symposium.