FRONTIERS IN regenerative medicine
Human stem cell growth in animal hosts might provide a new source of transplantable tissue.
When Juan Carlos Izpisua Belmonte and his team at Salk made global news headlines last fall for developing a technique for growing human stem cells within a mouse embryo, it no doubt puzzled the average reader. They may have asked:
What’s the point?
For the thousands of people waiting for life-saving organ transplants, the question would have been different:
When will this work?
T
That’s because Izpisua Belmonte’s discovery was a proof of concept for a potentially new source of transplantable organs, and for many patients that resource can’t come soon enough. Tens of thousands of people around the world receive organ transplants every year. But while the medical know-how for transplanting organs has expanded rapidly, the availability of donated organs has lagged. Due to the lack of donors and the risk of organ rejection, in the United States alone, an average of 22 people die each day while waiting for an organ donation.
Even for people who don’t require an immediate organ transplant to survive, chronic diseases can cause secondary health issues that could be prevented by replacing the damaged or diseased organ—for instance, the difficulty of managing insulin and blood sugar levels can result in diabetics going blind and losing limbs to amputation.

Against this backdrop, the rapid pace of stem cell science in recent years has provided a ray of hope. Scientists around the world have been exploring ways to use stem cells—cells still in nascent stages of development—to grow new tissues in the laboratory. Growing functional organs in the lab has, however, proved daunting. When a heart or a kidney forms in an animal during early development, it happens within the fetus, a complex environment that’s very difficult to recreate in a petri dish.
“We’re working every day on this problem of how to grow organs in the lab, but we’re still a long way away,” says Izpisua Belmonte. “But animals grow perfect organs all the time. It gave us the idea of using an animal as a host to grow a human organ.”
In a paper published in the journal Nature, the scientists reported they had been able to integrate human stem cells into early-stage mouse embryos so that the human stem cells began the first stages of differentiation—meaning they appeared to begin the process of generating precursors of the body’s various tissues and organs.
Researchers can now take a person’s skin cells, use chemicals to revert them back into what’s called induced pluripotent stem cells (iPSCs), and then coax those reprogrammed stem cells to turn into desired tissuespecific cells, such as those of the brain, muscle or pancreas.
Since then, with support from the Moxie Foundation, the Salk team has been exploring whether the same technique might allow pigs to be used as hosts for growing human organs. A key part of their approach is developing ways to precisely target the human cells to become specific organs needed for transplant. The Salk scientists have teamed up with experts in pig biology at the University of California, Davis; two universities in Spain, the Catholic University of Murcia and the University of Murcia; and the Spanish agricultural company, Agropor.
If their technique pans out, it could help overcome a major hurdle to organ transplants: the risk that the recipient’s body will reject the new organ. Several attempts have been made at transplanting whole animal organs into humans— the most famous of which was an American infant girl known as “Baby Fae,” who received a baboon’s heart—but patient immune systems inevitably reject the animal organs.
The Salk researchers think they may be able to get around this with advances in generating stem cells from patient cells that have already developed into a specific type of tissue, such as skin. Researchers can now take a person’s skin cells, use chemicals to revert them back into what’s called induced pluripotent stem cells (iPSCs), and then coax those reprogrammed stem cells to turn into desired tissue-specific cells, such as those of the brain, muscle or pancreas. If a person’s iPSCs were used to grow an organ in an animal, the organ might pose less risk for rejection because the cells have the same DNA as the original patient skin cell.
“If we can tell the human iPSCs in an animal host to develop into a kidney or pancreas or eye, it could provide an entirely new source for transplant tissues,” says Izpisua Belmonte. “We’re still in the initial stages of determining if this is even possible and whether human cells can participate in the early formation of tissues in the host animal and become part of their development. We have a long and exciting scientific problem ahead of us.”
Support a legacy where cures begin.
Featured Stories
 Frontiers in Regenerative MedicineWhen Juan Carlos Izpisua Belmonte and his team at Salk made global news headlines last fall for developing a technique for growing...
Frontiers in Regenerative MedicineWhen Juan Carlos Izpisua Belmonte and his team at Salk made global news headlines last fall for developing a technique for growing...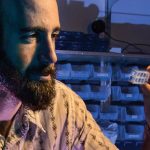 Next Gen: Zachary KatzZachary Katz is a visual person: from insect-devouring plants to bustling cells, he strives to see what happens in nature. While growing up in Arizona and then Florida, Katz and his brother gathered...
Next Gen: Zachary KatzZachary Katz is a visual person: from insect-devouring plants to bustling cells, he strives to see what happens in nature. While growing up in Arizona and then Florida, Katz and his brother gathered... An Interview with Salk President Elizabeth BlackburnWhen Jonas Salk announced the discovery of the polio vaccine in 1955, Elizabeth Blackburn was six years old and busy collecting...
An Interview with Salk President Elizabeth BlackburnWhen Jonas Salk announced the discovery of the polio vaccine in 1955, Elizabeth Blackburn was six years old and busy collecting...