Finding the "Secret Sauce" For Personalized, Functional Insulin-Producing Cells
For more than a decade, scientists across the globe strived to replace failing pancreatic beta cells linked to immune destruction in children (type 1 diabetes) or obesity-associated diabetes in adults (type 2 diabetes). Although cells made in a dish were able to produce insulin, they were sluggish or simply unable to respond to glucose.
“We found the missing energy switch needed to produce robust and functional human beta cells, potentially turning this discovery into a viable treatment for human diabetes,” says Ronald Evans, co-senior author and director of the Gene Expression Laboratory at Salk. The new work was published in Cell Metabolism on April 12, 2016.
Researchers uncover molecular switch to make effective sugar-responsive, insulin-releasing cells in a dish, offering hope for diabetes therapy.
The Salk technology begins with induced pluripotent stem cells (iPSCs), a technique where tissue from a patient is reprogrammed into other types of cells, such as from the pancreas. This step yields the pre-beta cells, which produce insulin but are not yet functional. While several research groups reached this juncture, the road forward to functional cells was not clear.
“Pancreatic beta cells must be able to do two things to work effectively: respond to glucose and produce insulin,” says Evans. “No one had been able to figure out how to make pancreatic cells from human patients that can do both until now.”
Eiji Yoshihara, first author and Salk research associate, together with Evans and Salk colleagues, closely studied the basic biology of a beta cell and uncovered several molecular switches, called transcription factors, that were switched off but might control the transition to a fully functional state. The “secret sauce,” the Salk team found, was one particular switch the Evans lab had studied for years for its role in cell signaling. This protein switch, called ERR-gamma, turned out to be crucial to awakening silent beta-like cells that could now respond to glucose and release insulin accordingly. The team found that when the matured beta cells were transplanted into type 1 diabetic mice, the procedure quickly rescued their diabetes.
“This advance will result in a better controlled insulin response than currently available treatments,” says Michael Downes, co-senior author and a Salk senior staff scientist. He adds that the team’s technique is an easy, fast and inexpensive way to make transplantable human pancreatic beta cells in a dish that genetically match patients. The researchers hope to move to human trials within the next few years.
Read News ReleaseFeatured Stories
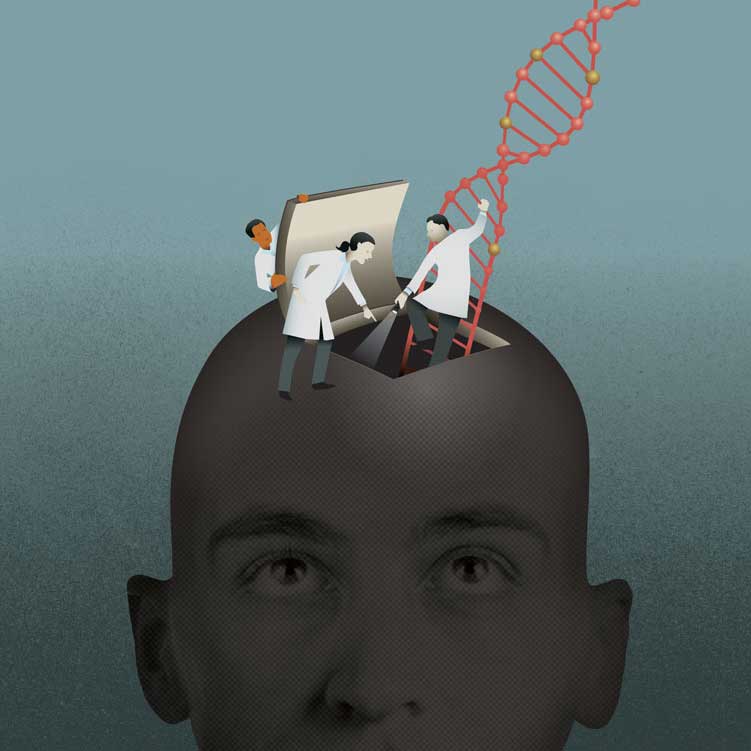 Beyond DNA: Unlocking the Secrets of the EpigenomeA layer of regulatory information on top of DNA is proving to be as important as genes for development, health and sickness.
Beyond DNA: Unlocking the Secrets of the EpigenomeA layer of regulatory information on top of DNA is proving to be as important as genes for development, health and sickness. Tapping our Immune System’s SuperpowerWe all have a superhero—or supervillian—inside our bodies. It’s called our immune system. Every day, a healthy immune system repels a host of adversaries—bacteria, viruses, parasites—you name it!
Tapping our Immune System’s SuperpowerWe all have a superhero—or supervillian—inside our bodies. It’s called our immune system. Every day, a healthy immune system repels a host of adversaries—bacteria, viruses, parasites—you name it! All about town with Pablo HollsteinGrowing up in Quito, Ecuador, Pablo Hollstein was passionate—and precise —about science from an early age.
All about town with Pablo HollsteinGrowing up in Quito, Ecuador, Pablo Hollstein was passionate—and precise —about science from an early age.