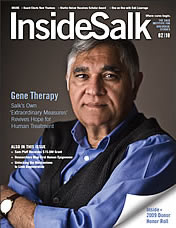
Jumping from theoretical physics to cancer research with no prior training in biological sciences wasn’t an easy transition for Gaurav Mendiratta. Couple this with a move across the world and the birth of his first child shortly after starting his postdoctoral training in a newly opened laboratory––Mendiratta had his work cut out for him.
“A month in, I picked up a pipette for the first time and had to learn how to culture stem cells,” Mendiratta recalls. “Naturally, the project was a complete mess, but I was learning. In science, we need to persevere to get anywhere.”
Born and raised in a small town near New Delhi, India, Mendiratta avoided the intense heat by spending the summers indoors playing with his favorite toy: a screwdriver. “My parents did buy me real toys,” he jokes. “But they wouldn’t last long because I would take them apart with my screwdriver to see how they worked.” No toy, radio or household appliance was safe from Mendiratta’s curiosity.
He carried this inquisitiveness into his high school years, where he’d spend countless hours studying for his favorite classes—math and physics. Although Mendiratta loved learning how logic and critical thinking could demystify real-world phenomena, his peers would tease him for being passionate about science.
“As a teen, I didn’t feel accepted by my classmates,” Mendiratta says. “But when I started hanging around academic circles, I realized there were others just like me. I wasn’t so strange after all!”
After high school, Mendiratta completed his bachelor’s degree at the University of Delhi, where his passion for quantitative reasoning blossomed. Upon graduation, he pursued his master’s in theoretical and mathematical physics and his doctoral degree in elementary particle physics at the Indian Institute of Science in Bengaluru (formerly called Bangalore), where he developed models to address long-standing questions in astrophysical dark matter.
Although Mendiratta found the work enthralling, toward the end of his doctoral program he began to see how
abstract his research was. “I realized that the theories I studied in particle physics were hard to test. They needed decades of planning and expensive equipment to even start exploring experimentally.”
In the final year of his studies, Mendiratta began consulting at a hospital in Bengaluru. He built a computational framework that used the body’s radioactive potassium concentration to noninvasively monitor a baby’s metabolism during pregnancy as well as metabolic states in cancer patients. “Being able to use my mathematical skills to explore equally complex systems in biology lit a fire in me,” says Mendiratta. “The idea of helping people got me hooked!”
In 2017, he started developing a mathematical model of tumor growth and immune system interactions, which he presented at several seminars. At the Southern California Systems Biology Conference at UC Irvine, he met his now mentor, Salk Assistant Professor Edward Stites.
“Meeting Ed at that conference was a stroke of good luck,” says Mendiratta. “He’s an MD/PhD, so he keeps our work clinically centered, but he was also a math major, so he speaks my language!”
At this fortuitous encounter, Mendiratta learned that Stites had just started a lab at Salk, where Stites and his team use computational and mathematical modeling to better understand complex protein interactions in cancer with the goal of offering patients more effective treatments. Mendiratta joined Stites’ lab as his first postdoctoral researcher, where he began applying his background in quantitative analysis to study the ways genetic mutations influence the development of cancer.
Mendiratta investigated how some cancer-associated genes and their mutations can be over- or underrepresented in some populations because of variability in sampling each type of cancer. Historically, only a handful of well-funded cancer centers have had the ability to sequence cancer patients’ tumor genomes. He found that this led to an inaccuracy in cancer data—the few patients who had access to these centers were not representative of cancer patients throughout the rest of the US.
“This oversight prompted us to better account for the population of patients seen across the country when calculating gene mutation rates in cancer,” says Mendiratta.
To address this issue, he helped develop a new classification tool called ROSETTA, along with a method to pool cancer data and statistics from several databases. This work provides researchers, clinicians and policymakers with a better understanding of the incidence of cancer-related gene mutations within US populations, a key step for evaluating resource allocation and research priorities to achieve the best outcomes for cancer patients.
Mendiratta and Stites are also applying their mathematical expertise to piece together a major puzzle in treating melanomas—certain treatments that reduce tumor size inadvertently lead to the formation of a second tumor.
They created a computer-based simulation to model the interactions between the cancers and the drugs, and discovered complex molecular reactions that were previously unaccounted for, findings that could aid efforts in diagnosing and treating melanomas.
“Computational modeling can help us solve some of the hardest biological problems,” Mendiratta says. “Because when we think quantitatively, we’re throwing the darts with a clearer view of the board, which gives us a better chance of hitting the bull’s-eye.