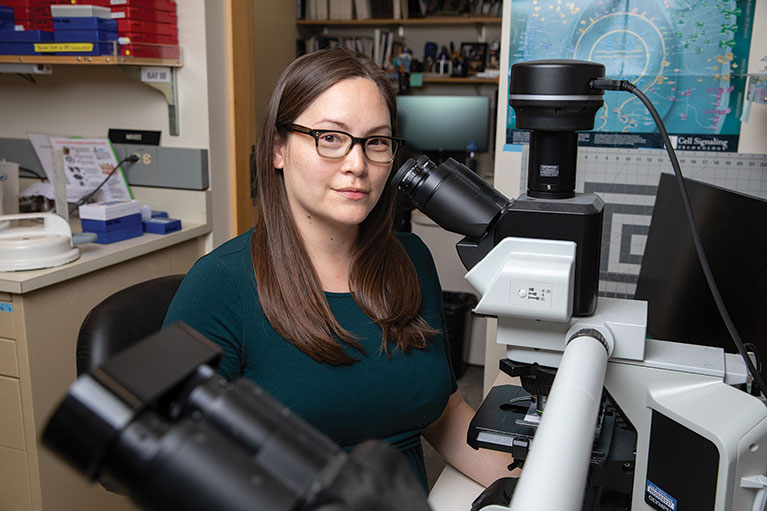
Observations Dannielle Engle Putting patients first
Assistant Professor Dannielle Engle has a deeply personal connection to pancreatic cancer that changed her career trajectory and made her want to focus on the disease’s early detection and treatment.
Inside Salk sat down with Engle to find out more about her dedication to finding better treatment options for people with pancreatic cancer and its precursor, pancreatitis (inflammation of the pancreas).
The pancreas is an abdominal gland that makes digestive enzymes and hormones, including insulin. Because the early symptoms (bloating, fatigue, nausea) are common to many conditions, pancreatic cancer—the third-leading cause of cancer deaths in the United States—is often not diagnosed until later stages, when treatment options, such as surgery, are limited or ineffective.
Engle’s work is already proving to be so groundbreaking that it is garnering such prestigious awards as the first Lustgarten Foundation-American Association for Cancer Research Career Development Award for Pancreatic Cancer Research, in Honor of Ruth Bader Ginsburg, the late Supreme Court Justice and women’s rights pioneer who lost her life to the disease.
You have a personal connection to pancreatic cancer. Would you please share it with us?
DE: When I was a senior in college, my father was diagnosed with pancreatic cancer. At first it seemed he was very lucky because he developed an early warning sign called jaundice, a condition that causes your skin to turn yellow. He was diagnosed with stage 1 pancreatic cancer, so he was eligible for surgery. It’s a very complicated surgery, with a mortality rate of upward of 10 percent. So, I flew home to be with him and the rest of our family. The surgeons removed the tumor, but every single one of his lymph nodes was positive. What that means is, he actually had metastatic pancreatic cancer that had spread to his lymph nodes. What we thought was stage 1 was actually stage 4—the most advanced stage. Even in the luckiest scenario, we were still left with very few options. He died 14 months later. That was hard. I still get emotional every time I talk about it.
How did your father’s diagnosis change your career trajectory? Weren’t you studying music in college?
DE: Yes, I had always liked both and was pursuing a music major and a biology minor. But at some point, I was no longer satisfied. I had this intellectual drive and curiosity about science. And in conversations with my dad, he had said, “Certainly you bring joy to people’s lives by playing music. But, you know, clinicians are making patients feel better. And scientists are figuring out why they’re sick in the first place, and how to prevent it from happening. That’s a level of impact that few people have an opportunity to make.” Then my first experience in a lab helped me make the decision. I thought, “I could do this every day of my life and be completely fulfilled.” That’s when I realized that I will always love music, but science is really my calling.
What did you do next?
DE: I completed my PhD in biological sciences and started my postdoctoral research in David Tuveson’s lab, which is the eminent lab focusing on pancreatic cancer. A few years into my fellowship, my uncle—my mother’s brother—was diagnosed with pancreatic cancer. He died six months later. That was a punch in the gut because I’m studying pancreatic cancer, but I’m not finding answers fast enough; I still don’t know enough.
I realized what we need is more labs completely dedicated to studying pancreatic cancer because this is the reality for most people diagnosed with pancreatic cancer. You hear about those tremendously lucky cases like Ruth Bader Ginsburg, who survived more than 10 years. But how did we find her pancreatic tumor? It’s because she was being surveilled for colorectal cancer relapse; she was receiving regular scans, and they found this tiny tumor in her pancreas before it spread—and it still got her 10 years later!
How do you find motivation in the face of such overwhelming odds?
DE: I used to attend research walks and awareness campaigns and would never meet a pancreatic cancer survivor. But we had a research walk last spring, and I met three survivors. I didn’t have to search for them; I didn’t have to scour the social media networks for them; they were just there. And it’s so encouraging. There is scientific progress, it’s just still slow. But the work is leading to new drugs.
In 2019, you made a pretty significant discovery—that a carbohydrate molecule called CA19-9, which is present on many proteins, causes the progression from pancreatitis to pancreatic cancer. Can you talk about that?
DE: CA19-9 is expressed in pancreatic tumors, and we previously thought it didn’t really do anything, that it was just an inert bystander. But CA19-9 is actually secreted and travels systemically throughout the body. I found that it’s a signaling molecule that affects both the immediate environment of the pancreas as well as the surrounding microenvironment through its interactions with fibroblasts—connective tissue cells—and macrophages, a type of immune cell.
Your lab is doing both basic research and testing new drugs, correct?
DE: Most research starts with understanding normal biology and how it’s perturbed in disease, whether that’s inflammation—pancreatitis—or pancreatic cancer. And then that mechanistic understanding gives us targets, and we can chase after those targets to see if they would be good biomarkers for early detection or drug development. Our lab starts with the normal biology and goes all the way to clinical applications.
“Certainly you bring joy to people’s lives by playing music. But, you know, clinicians are making patients feel better. And scientists are figuring out why they’re sick in the first place, and how to prevent it from happening. That’s a level of impact that few people have an opportunity to make.”
– Assistant Professor Dannielle Engle
Can you explain what a patient organoid model is?
DE: A patient organoid model is a living avatar that mimics the characteristics of the tumor or diseased tissue from which it is derived. We use these models in several different ways. This includes understanding the underlying reasons for why tumors are resistant to treatment and how they interact with local microenvironments. And, in addition to doing the traditional research work, we also do what’s called a “tumor board,” where we very rapidly try to find a drug treatment that works for a specific patient. Right now, we do this empirically, testing drugs one by one. But in the future, we hope that we can make this process faster by finding predictive biomarkers. For example, if a patient’s organoid model expresses markers X, Y, and Z, they’re more likely to respond to treatments A and B. Whereas if they don’t express those three markers, and instead express completely different markers, they’re more likely to respond to treatment C or to something else.
In addition to studying cancer, our lab has been creating a human biobank of pancreatitis organoids—essentially, pancreases in a dish—to better understand the progression from inflammation to cancer. Very little is known about human pancreatitis in terms of cell signaling and its interactions with the microenvironment because it’s hard to study.
Now that we have these renewable organoid models, we can do mechanistic dissections that we’ve done for normal and tumor biology in this intermediate inflammatory stage.
We’re leveraging what we’re good at—drug testing, pharmacotyping (defining patient variability in drug testing), and precision medicine approaches for cancer—and we’re bringing that to bear on pancreatitis because it’s a debilitating disease. It’s interesting not just because it’s a risk factor for
pancreatic cancer but also because it affects millions of people and is incredibly painful. Hopefully in the next few years we’ll be able to add some additional treatment options. (For more about Engle’s organoids, see Frontiers.)
At Salk, you’re now serving as a pancreatic organoid resource for labs around the world. How does that feel?
DE: The beautiful thing about the Salk Institute is that we’re not here to be famous or to be the sole expert in some area and defend our turf. It’s about working together to ask bigger, more transformative questions.
We are incredibly collaborative in the pancreatic cancer field. I was trained in an environment where you are generous—because guess what? We’re never going to run out of questions. It’s not like there are only 10 questions in the world that are important, and we have to compete over them.
And being personally affected—having lost my father and my uncle—for me it’s not a matter of who’s right. It’s a matter of getting better care for our patients. And so that requires that you take a step back and that you don’t let your ego come into play, because we’re better scientists when we have diverse perspectives, and when we collaborate—the ideas are just exponentially better.
You’ve garnered a good deal of financial support for your lab over the past few years. What has that allowed you to do?
DE: The first thing the funding enabled me to do is build a spectacular team. I currently have three postdoctoral researchers, three graduate students, and four research assistants. We work on every single stage of pancreatic disease, from the first episodes of inflammation that open the gateway to formation of tumors to metastasis, which is what most patients actually die from.
The lab has really grown over the years, with a sense of camaraderie as well as independence. It’s been rewarding to see the team take existing projects and make them their own, but also establish projects based off of their own ideas. I think, as a new principal investigator, that was one of my first worries—I think they get along; are they going to work well together? But, you know, when you have a diverse group of people who all have this common goal and common work ethic, it’s really, really cool to see them blossom as a team.
You’re committed to ensuring diversity in your lab and more generally. Can you talk about that?
DE: Diversity is incredibly important to me. I started my lab with a mission to help patients with pancreatic cancer, but I also wanted to help scientists in my lab be both better scientists and better people. That requires being in a diverse environment. When we have different ways of thinking, that’s when the most transformative ideas come about. Granted, the whole world has a lot of work to do, but here at Salk, it’s our mission to be excellent in everything, and diversity is included in that mission. Our founder, Jonas Salk, recognized that when he said, “It’s our responsibility to be good ancestors.” I think that is what he meant.
Support a legacy where cures begin.
Featured Stories
 Leading with Technology – Salk scientists develop new means of discoveryOur scientists continue to push technological limits to—among other things—store more excess atmospheric carbon in deeper plant roots, study pancreatic cancer more accurately, follow cellular activity in real time more clearly, and track all kinds of motion more easily.
Leading with Technology – Salk scientists develop new means of discoveryOur scientists continue to push technological limits to—among other things—store more excess atmospheric carbon in deeper plant roots, study pancreatic cancer more accurately, follow cellular activity in real time more clearly, and track all kinds of motion more easily. Dannielle Engle—Putting patients firstEngle, an assistant professor, has a deeply personal connection to pancreatic cancer that changed her career trajectory and made her want to focus on the disease. Inside Salk sat down with Engle to find out more about her dedication to finding better treatment options.
Dannielle Engle—Putting patients firstEngle, an assistant professor, has a deeply personal connection to pancreatic cancer that changed her career trajectory and made her want to focus on the disease. Inside Salk sat down with Engle to find out more about her dedication to finding better treatment options.
 Weiwei Fan—Life is energyFan, a staff scientist in Professor Ronald Evans’ lab, studies mitochondria because he feels drawn to understanding how these energy generators within our cells function and the natural variations that exist between individuals.
Weiwei Fan—Life is energyFan, a staff scientist in Professor Ronald Evans’ lab, studies mitochondria because he feels drawn to understanding how these energy generators within our cells function and the natural variations that exist between individuals. Natanella Illouz-Eliaz—Recipe for a plant biologist: tomatoes, failure, and perseveranceIllouz-Eliaz, a postdoctoral researcher in Professor Joseph Ecker’s lab, grew up in Israel near the border with Lebanon, where high-pitched sirens periodically drove her family into bomb shelters for safety. But her parents insisted that she get the best education possible.
Natanella Illouz-Eliaz—Recipe for a plant biologist: tomatoes, failure, and perseveranceIllouz-Eliaz, a postdoctoral researcher in Professor Joseph Ecker’s lab, grew up in Israel near the border with Lebanon, where high-pitched sirens periodically drove her family into bomb shelters for safety. But her parents insisted that she get the best education possible. Richard Heyman—From Salk to biotech and backHeyman, a scientist and entrepreneur who has founded numerous biotechnology companies, currently serves as vice chair of Salk’s Board of Trustees, but his Salk story actually began when he was a postdoctoral researcher in the lab of Professor Ronald Evans.
Richard Heyman—From Salk to biotech and backHeyman, a scientist and entrepreneur who has founded numerous biotechnology companies, currently serves as vice chair of Salk’s Board of Trustees, but his Salk story actually began when he was a postdoctoral researcher in the lab of Professor Ronald Evans.