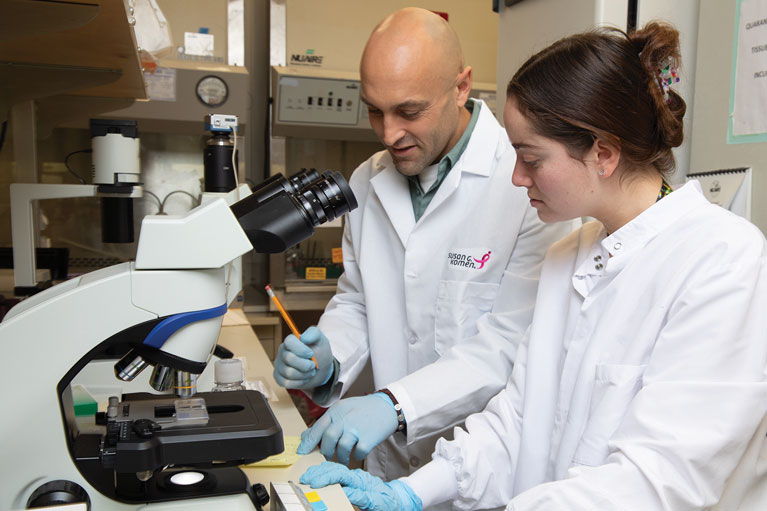
Observations Daniel Hollern Turning a cancer diagnosis into a career in basic research
Assistant Professor Daniel Hollern pivoted his career trajectory after a family member’s life-changing diagnosis pushed his already-curious mind off a cliff of questions—starting with, “What can I do to help him?”
Inside Salk sat down with Hollern to uncover the details of his journey from Michigan to California, and where—along the way—he got his start as an immunologist chipping away at cancer’s fundamental processes.
Hollern looks at how the immune system and triple-negative breast cancer interact, asking where and why the immune system fails to recognize and destroy cancerous cells.
He’s currently focused on the immune system’s B cells, which he is trying to program to paint targets on cancer cells to promote their destruction.
Hollern has already earned numerous awards for his cancer research efforts, including an Aitch Foundation Award, two National Institutes of Health Ruth L. Kirschstein National Research Service Awards, a Joseph S. Pagano Award, a Metavivor Award, a California Breast Cancer Research Program Award, and a Susan G. Komen grant. Still early in his career, these honors mark the beginning of a lifetime of discovery to come.
When did you first become interested in science?
DH: I was the oldest of seven kids, so one of the things my mom did to calm the chaos a bit was allow us to take all the spices, vinegar, and baking soda to create concoctions and “play science.” I would argue that it wasn’t totally scientific at the time, but it really got me started being creative and using my imagination in a scientific way.
I really started enjoying science in high school, since I saw it going hand in hand with sports. At first, I wanted to be an orthopedic surgeon because I had sports injuries. That started me thinking about human health, what’s going on underneath the hood, and how we might fix things in our bodies.
When did you make the transition from orthopedic surgery to cancer biology?
DH: I was really focused on this orthopedic surgery career path all the way until my grandfather was diagnosed with cancer while I was in college. And when I found out what type of cancer he had, I’d never heard of it. It was angiosarcoma in his scalp. I started to learn a lot about it because my grandfather was my best friend. He was my anchor, and seeing what was going to happen to him with no treatment options just really devastated me and started to get me thinking, “What can I do to help him?”
So, I started to read the scientific literature that’s out there and realized I needed to go into basic research to start to tease apart what’s happening in these cancer patients. What’s limiting their therapeutic options? What options do they have if their tumors aren’t showing specific markers for an available treatment? What can we do for those people? Since changing my major as an undergrad, I’ve been entirely focused on this mission.
And once you decided on basic research, did those childhood kitchen experiments translate to lab skills?
DH: I enjoyed lab work, but I was not skilled coming into the lab. In fact, that was one of the things that I remember telling my eventual mentor when I interviewed with him. I only had one semester of undergraduate independent research experience. I had one technique under my belt. And so what I told him is, “I have a lot to learn, but you’ll never find somebody that will work as hard as me to achieve the goals of your laboratory and to learn these methods that you’re using to take apart cancers to discover why it exists in people’s bodies and why it’s so hard to contain.”
What kinds of methods and techniques have you used since then?
DH: Back then, I trained a lot in a method called bioinformatics, where we sequence tumors and learn what instructions they’re using that are sustaining the cancer. Then, we can look at those instructions and see where we can manipulate or interrupt that pathway to cancer growth.
Technology has advanced so much now that it’s hard to even keep up with the new platforms. Luckily, at Salk we have these advanced technologies and the resources available to maximize their impact. What these modern technologies allow us to do is take a part of a tumor, while simultaneously looking at the patient’s immune system function—that way we can identify exactly what is going wrong between the two.
Now that you’re at Salk, what sorts of projects are you working on?
DH: We’re trying to understand what the dysfunctions are in a patient’s immune system that prevent it from eliminating cancer. It’s estimated that every single day, we have cancer cells arise in our bodies and our immune system takes care of them. We want to see why and where this process is going wrong in people with cancer, then try to hardwire it to start working right.
What’s amazing about doing this is we can see that we can actually cure tumors without chemotherapy by just solving those problems in the immune system, so it recognizes and attacks cancer again. And we are currently focused on triple-negative breast cancer, which is a type of breast cancer that doesn’t have the three most common breast cancer receptors that established therapies target, in turn making it much more difficult to treat.
What’s important about the research we’re doing in triple-negative breast cancer is that it’s one of the most complex and challenging tumor types to cure with immunotherapies. So, what I really envision is, as we start to establish the fundamental principles of how to activate an immune response against these tumors, we’ll see those principles translate to other cancer types that have those same challenges.
“Soon enough, cancer is not going to be this impossible-to-cure disease. […] [That] keeps me motivated and makes everyone in my lab feel like we’re chasing something important that will translate to patient care.”
–Daniel Hollern
What part of the immune system most interests you?
DH: We’ve identified B cells as a really important cell in the immune system when it comes to cancer. The reason that B cells are so important for developing new cancer immunotherapies is that they are capable of basically painting a target on any type of tumor cell to mark it for destruction by the immune system. And one of the ways B cells do this is through the production of antibodies, which are large proteins that function as that “bulls-eye” for our immune system to go after.
What is amazing is these protective antibodies cover every extracellular surface. What we’re trying to do with cancer is really use these B cells to paint targets on cancer cells, amplify an immune response against it, and cause that curative response that patients need.
Is there a reason you look at breast cancer over another cancer type, like the one your grandfather had?
DH: They had a really strong breast cancer research program at Michigan State University, where I did my PhD. And I realized, if we’re trying to solve cancer and we appreciate that everybody’s cancer is unique, that patient-to-patient variation is very present in breast cancer. So, if I learn those fundamentals and how to do the research within breast cancer, then I’m going to be able to pivot and attack the angiosarcoma that killed my grandfather. That’s something that I’m aiming to do
here at Salk.
Which of your recent discoveries do you find the most exciting?
DH: We’re really focusing on figuring out how to hardwire a B cell response to kill every single cancer cell that’s in a tumor. B cells are a unique solution to the challenges that cancer is presenting us with. Once we identify the way B cells can be manipulated to target cancer, which is what we’re focused on in my laboratory, we envision that we’re going to be able to ensure that every patient’s immune system is responding in a way that targets all of the cancer cells and allows them to survive this disease.
The fundamentals are becoming more and more clear as to how we correct those immune system imbalances. Soon enough, cancer is not going to be this impossible-to-cure disease. Instead, you’re going to need treatment, but you’re going to survive. Your life expectancy is not going to change. And that is just such an exciting and hopeful place to be in that it wasn’t imaginable even when I started graduate school. It keeps me motivated and makes everyone in my lab feel like we’re chasing something important that will translate to patient care.
Do you collaborate often with other Salk labs?
DH: Yes, we collaborate with other faculty and are so inspired by their research. I have never experienced such a transformative time in my life, where my perspective developed and broadened any faster or more. When I came to Salk and started to interact with the scientists here, I started to think, “Okay, in my laboratory, if this is true, how do I apply this concept, and what are the important directions to start to go in?” Other faculty have been one of the crucial components in creating our sense of confidence that we can really attack this disease effectively, because we gain inspiration and hope from their discoveries, and we are in that sort of environment where inspiration is happening pretty much on a daily basis.
Support a legacy where cures begin.
Featured Stories
 Interaction + Infrastructure = Innovations in Healthy AgingSalk formula recalculates aging research, shifting focus to overall resilience and health span.
Interaction + Infrastructure = Innovations in Healthy AgingSalk formula recalculates aging research, shifting focus to overall resilience and health span. Salk mourns the loss of Nobel Laureate Roger GuilleminThe Institute remembers the “father of neuroendocrinology” for his many contributions to science and friendship to all.
Salk mourns the loss of Nobel Laureate Roger GuilleminThe Institute remembers the “father of neuroendocrinology” for his many contributions to science and friendship to all. Professor Jan Karlseder named Salk’s Chief Science OfficerOn February 1, Jan Karlseder started as Salk’s new senior vice president and chief science officer (CSO).
Professor Jan Karlseder named Salk’s Chief Science OfficerOn February 1, Jan Karlseder started as Salk’s new senior vice president and chief science officer (CSO).  Daniel Hollern–Turning a cancer diagnosis into a career in basic researchAssistant Professor Daniel Hollern pivoted his career trajectory after a family member’s life-changing diagnosis pushed his already-curious mind off a cliff of questions—starting with, “What can I do to help him?”
Daniel Hollern–Turning a cancer diagnosis into a career in basic researchAssistant Professor Daniel Hollern pivoted his career trajectory after a family member’s life-changing diagnosis pushed his already-curious mind off a cliff of questions—starting with, “What can I do to help him?” Jerry Sheehan–Collaborating shoulder to shoulder with scientistsWhen you think about a person who heads an information technology department, you might not envision them working shoulder to shoulder with research scientists. But that’s exactly the approach Jerry Sheehan is taking as Salk’s new chief information officer (CIO).
Jerry Sheehan–Collaborating shoulder to shoulder with scientistsWhen you think about a person who heads an information technology department, you might not envision them working shoulder to shoulder with research scientists. But that’s exactly the approach Jerry Sheehan is taking as Salk’s new chief information officer (CIO). Laura Mainz–Taking control after a cancer diagnosisLaura Mainz grew up in a tiny village in midwestern Germany, with just as many cows as people. But the sweeping landscape speckled with farms never swayed her toward plant biology—instead, her interest in the human body grew.
Laura Mainz–Taking control after a cancer diagnosisLaura Mainz grew up in a tiny village in midwestern Germany, with just as many cows as people. But the sweeping landscape speckled with farms never swayed her toward plant biology—instead, her interest in the human body grew. Black Association affinity group cultivates welcoming environmentThe Black Association at Salk (BAS) was one of the first affinity groups formed at Salk in 2020. Since that time, it has established itself as a welcoming space and go-to for resources for all Black Salk community members.
Black Association affinity group cultivates welcoming environmentThe Black Association at Salk (BAS) was one of the first affinity groups formed at Salk in 2020. Since that time, it has established itself as a welcoming space and go-to for resources for all Black Salk community members.