New COVID-19 Research Projects
COVID-19 FEATURE
In addition to Salk’s ongoing research areas relevant to COVID-19, several new coronavirus-specific projects have recently launched. These innovative projects range from understanding the structure of the virus to mobilizing the body’s immune reaction.

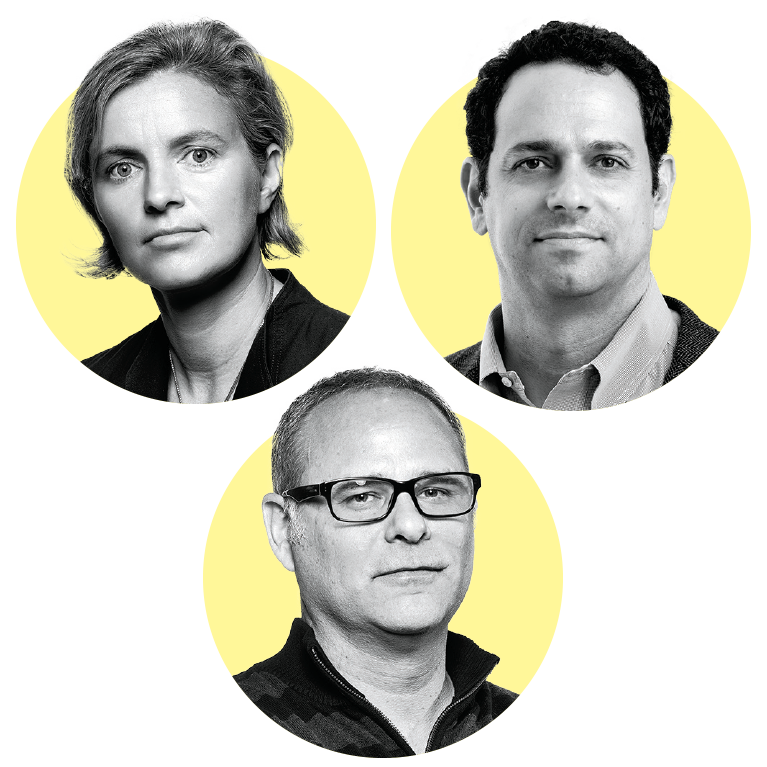
Tony Hunter & Gerald Pao
In severe COVID-19 cases, immune cells in the infected windpipe and lungs can release high levels of damaging inflammatory proteins called cytokines, colloquially known as a “cytokine storm.” American Cancer Society Professor Tony Hunter previously showed that the cytokine LIF (leukemia inhibitory factor) plays a role in pancreatic cancer. He will test whether cytokines, like LIF, play a role in the immune overreaction seen in some COVID-19 patients.
Gerald Pao, a staff scientist in the Hunter lab, will work with the Sanford Burnham Prebys Medical Discovery Institute to generate a virus system that expresses a spike protein that mimics the ones on the coronavirus. The team will then examine the immune response to these spike proteins.
In collaboration with UC San Diego, USC and Sanford Burnham Prebys Medical Discovery Institute, Pao will develop a test to detect the presence of COVID-19 genomes in human nose and throat samples. He has designed this test, which will combine CRISPR with an imaging technology, so that it will only take a few minutes.
Pao will also engineer CAR-T cells, cells that can target specific proteins, to aid in the development of a coronavirus vaccine. These cells are repurposed from cancer immunotherapy to provide immune surveillance and kill coronavirus-infected lung cells that have a spike protein on their surface, early in the infection.
Clodagh O’Shea, Alan Saghatelian & Joseph Noel
It will take a virus to kill a virus. Professors Clodagh O’Shea, Alan Saghatelian and Joseph Noel are exploiting the atomic structures of the SARS-CoV-2 virus, together with proprietary synthetic virology and chemical biology platforms, to create transformative vaccines and gene therapies. Their pipeline will target i) SARS-CoV-2 prevention by creating synthetic live viral vaccines that induce broad and long-lasting immunity and ii) SARS-CoV-2 treatment through viral gene therapies that express synthetic nanoparticles that seek, neutralize and destroy SARS-CoV-2 and prevent pathology. This research will uncover underlying principles and overcome intractable clinical challenges, not just of SARSCoV- 2 today, but of SARS-CoV-3 tomorrow.

Susan Kaech
Professor Susan Kaech, who studies how we develop immunity to severe viral infections, such as influenza and now COVID-19, will collaborate with The Scripps Research Institute and La Jolla Institute to study the types of memory T and B cells that form in the lung following SARS-CoV-2 infection as a way to understand if and how long-term immunity can be established. This work will be critical to understanding the types of memory T cells that COVID-19 vaccines will need to re-create in vaccinated individuals to establish benchmarks for generating protective immunity.
Creating a protective coronavirus vaccine is currently one of the world’s greatest challenges. Kaech believes that immune cells called memory B and T cells are likely critical for controlling the infection, and could therefore be excellent targets for vaccines to enable long-term immunity. Her lab, in collaboration with The Scripps Research Institute, will examine the role of memory T cells inside the lungs during a COVID-19 infection.
In a separate study, in collaboration with pulmonary physicians at UC San Diego and the VA hospital, Kaech will examine changes in the levels and composition of surfactant in COVID-19 patients. Surfactant is a substance in the lungs that allows us to breathe. The study will compare surfactant levels with the health outcomes of COVID-19 patients to determine if a drop in surfactants is associated with more severe disease. Her lab will also test if genetic alterations in pathways that control surfactant levels in the lungs alter the course of the disease.
Dmitry Lyumkis
Assistant Professor Dmitry Lyumkis will examine the molecular mechanisms by which the non-structural protein NSP1 halts host protein production. This process ultimately helps the virus in promoting the production of its own viral proteins and the development of COVID-19.
The Lyumkis lab will also explore how the non-structural protein NSP2 affects host cells during the development of COVID-19.


Juan Carlos Izpisua Belmonte
Professor Juan Carlos Izpisua Belmonte is collaborating with a San Diego biotechnology company to develop COVID-19 treatments using nanoparticles. The researchers will use RNA-targeting CRISPR-Cas technology to destroy the SARS-CoV-2 virus’ RNA. This treatment will prevent the virus from replicating in the body, thereby reducing the severity of an individual’s COVID-19 infection and limiting the virus’ chances
Support a legacy where cures begin.
Featured Stories
 Apart but togetherAs COVID-19 spreads across the world, organizations like the Salk Institute have mobilized to respond. In this feature article, read about how the Institute is adapting and continuing its groundbreaking science.
Apart but togetherAs COVID-19 spreads across the world, organizations like the Salk Institute have mobilized to respond. In this feature article, read about how the Institute is adapting and continuing its groundbreaking science. New COVID-19 research projectsIn addition to Salk’s ongoing research areas relevant to COVID-19, several new coronavirus-specific projects have recently launched. These innovative projects range from understanding the structure of the virus to mobilizing the body’s immune reaction.
New COVID-19 research projectsIn addition to Salk’s ongoing research areas relevant to COVID-19, several new coronavirus-specific projects have recently launched. These innovative projects range from understanding the structure of the virus to mobilizing the body’s immune reaction.
 A conversation with Martin HetzerIn the last few months, Salk Vice President and Chief Science Officer Martin Hetzer spearheaded the Institute’s efforts to respond to the pandemic from both an administrative as well as a scientific perspective.
A conversation with Martin HetzerIn the last few months, Salk Vice President and Chief Science Officer Martin Hetzer spearheaded the Institute’s efforts to respond to the pandemic from both an administrative as well as a scientific perspective.
 Eiman Azim – Decoding dexterityIn this Q&A, Assistant Professor Eiman Azim shares his thoughts on what’s next in neuroscience, how all scientists are philosophers and what he learned about movement from observing his newborn.
Eiman Azim – Decoding dexterityIn this Q&A, Assistant Professor Eiman Azim shares his thoughts on what’s next in neuroscience, how all scientists are philosophers and what he learned about movement from observing his newborn.
 Nasun Hah – Next gen sequencingAs the director of the Next Generation Sequencing Core, Staff Scientist Nasun Hah collaborates with everyone from plant biologists to neuroscientists to provide support and information about sequencing genes and entire genomes.
Nasun Hah – Next gen sequencingAs the director of the Next Generation Sequencing Core, Staff Scientist Nasun Hah collaborates with everyone from plant biologists to neuroscientists to provide support and information about sequencing genes and entire genomes. Update on initiatives to support diversity and BIPOCLearn about the Institute’s commitment to and actions around diversity and inclusion.
Update on initiatives to support diversity and BIPOCLearn about the Institute’s commitment to and actions around diversity and inclusion. Molly MattyMolly Matty, a postdoctoral researcher in the lab of Associate Professor Shrek Chalasani, shares what worms can teach us about human behavior, why science outreach is so important and why she enjoys puns.
Molly MattyMolly Matty, a postdoctoral researcher in the lab of Associate Professor Shrek Chalasani, shares what worms can teach us about human behavior, why science outreach is so important and why she enjoys puns.